COVID-19 face masks
by The independent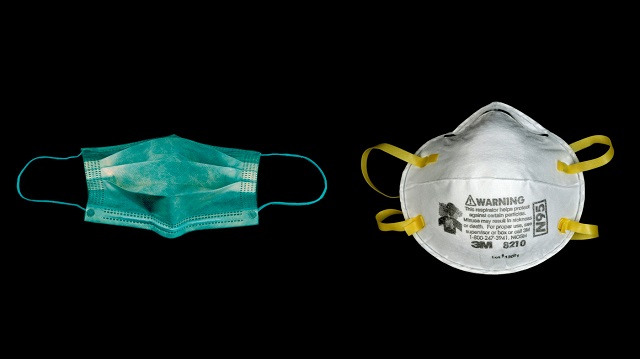
It’s critical for the public to be aware of limitations of wearing masks to avoid infection risk and false security
ANALYSIS | DR. BRUCE TUMWINE RWABASONGA | President Museveni on May 19 extended the national lockdown due to COVID-19 and announced that the government planned to procure and issue face masks to every Ugandan above the age of six years. The use or nonuse of face masks by healthy people in public to prevent the spread of COVID-19 has been one of the most confusing and contentious subjects amongst public health experts since the outbreak started.
For example, as recent as late February 2020, the Surgeon General of the U.S. (who by default is the government’s leading spokesman on public health) was tweeting ‘seriously people –stop buying masks…’ only to later change this stance after the CDC issued recommendations in late April encouraging use of face masks by healthy people in public to prevent COVID-19 transmission.
To date, the WHO only recommends use of face masks for COVID-19 protection amongst healthy people only if they are caring for someone with a COVID-19 diagnosis or if they are coughing or sneezing themselves.
The reason why the policy and guidelines on this policy have been confusing and contentious goes beyond scientific reasons. A lot of considerations have to be made before enacting such a policy. Some of these considerations include the culture of the region and likelihood to adopt the policy, access and prioritisation of resources needed and if the policy is re-enforceable or not.
All this leads to a couple of important questions.
- Should Uganda adopt the public health policy on mandating use of face masks in public by healthy people to prevent COVID-19 transmission?
- If so, is the policy of procuring and issuing a face mask to every single Ugandan above the age of six the optimal implementation strategy?
While the response to question 1 is slightly easier to answer, question 2 is more nuanced and complex because of the following.
While it remains to be seen what kind of masks will be issued by the government to the public, the effectiveness of masks depends on a myriad of factors, foremost of which is the design and materials that the mask is made of. Assuming that the government follows CDC guidelines and issues low cost cloth masks instead of surgical masks and N-95 respirators, which are currently being rationed for healthcare workers, it will lead to an obvious question. Why did the Ugandan government unlike other governments decide to procure and issue masks instead of focusing just on policy re-enforcement?
An article published in the American Chemical Society in April 2020, showed that improper fitting of cloth masks can lead to gaps between the mask and the face which can result in over 60% decrease in the filtration efficiency. This essentially implies that manufacturers when making cloth masks, need to tailor the mask to the wearer so as to minimize issues of mask ‘fit’ and leakage while allowing the exhaled air to vent efficiency. For this reason alone, it doesn’t make sense for the government to procure generic ‘one size fits all’ masks instead of letting individuals procure those that are tailor made for them. This reason alone would make this idea a non-starter, that is even before considering the manufacturing, distribution and supply chain nightmare that the government will ultimately experience before the end users receive these masks.
Secondly, the effectiveness of any tool or resource depends on user proficiency or lack thereof. Likewise, the effectiveness of masks in prevention of COVID-19 will depend a lot on how the end users use them. As clinicians know or as the public has seen on internet memes or with celebrities wearing a face mask, it is not as straightforward as many would assume. Many wearers while wearing the mask, unassumingly either don’t cover the mouth or the nose which significantly decreases its effectiveness. Worse still, poorly removing or placing the face mask by touching the piece over the mouth or nose instead of the straps, might actually increase the risk of COVID-19 transmission!
Furthermore, research findings in an article published in the British Medical Journal (BMJ) showed that moisture retention, reuse of cloth face masks and poor filtration could potentially result in increased risk of infection. Therefore, as the government implements this policy, public health sensitisation will be critical to ensure effective face mask use, removal and disposal so as to prevent face masks from being a vector of the infection.
In theory, the biggest risk that this policy might cause is creation of a false sense of security and the resultant decreased adherence to other prevention measures like social distancing etc. The BMJ article referenced above is also one of the few cluster randomised trials to compare the efficacy of cloth face masks to medical masks. Unfortunately, it showed that the cloth masks were much less efficacious than medical masks, penetration of cloth masks by particles was almost 97% while that of medical masks was 44%. Therefore, it is critical for the public to be aware of the limitations of wearing masks and to continue practicing other COVID-19 prevention strategies.
In conclusion, while the public health policy of mandating use of face masks in public by healthy people to prevent COVID-19 transmission is potentially an effective policy, there are lots of hurdles that the government will have to overcome.
Public education and improvement of the population’s health literacy on COVID-19 are some of the key factors on whether or not this policy will succeed. In addition to conducting public health campaigns on optimal face mask use, removal and disposal, the government needs to continue to emphasise the other COVID-19 prevention strategies; social distancing, minimizing public trips to only essential ones, not touching the face, washing hands etc.
****
Dr. Bruce Tumwine Rwabasonga, MBChB,MPH,MHA is a physician, public health professional and health services consultant based in Washington, DC.
Email: mande166@umn.edu
CLICK TO READ ONLINE MAGAZINE HERE
Share on: WhatsApp