Study finds very low level of SARS-CoV-2 in two San Francisco Bay areas
by Dr. Liji Thomas, MDA new study published on the preprint server medRxiv* in May 2020 reports a very low prevalence of antibodies in two separate populations living in the San Francisco Bay Area.
Coronavirus disease 2019 (COVID-19) is a new pneumonic illness that is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This disease is rapidly transmitted, causing a spectrum of disease from asymptomatic infection to acute respiratory distress syndrome (ARDS), which is frequently fatal. The relatively high morbidity and mortality rate of this pandemic have caused a heavy, sometimes overwhelming burden on health systems all over the world.
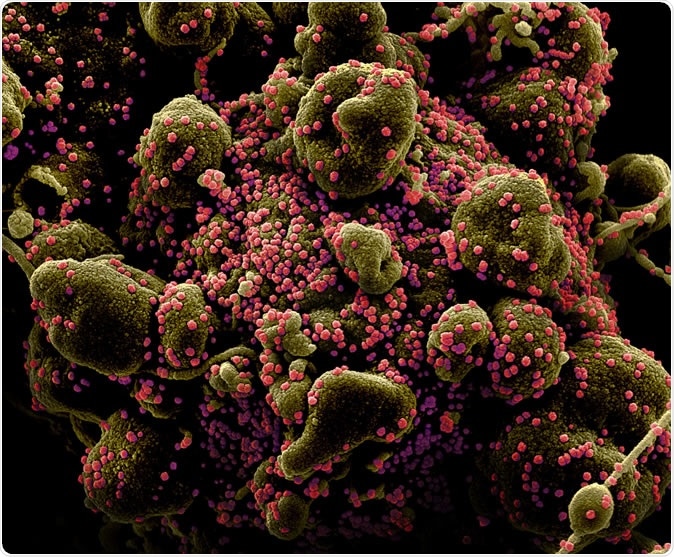
Novel Coronavirus SARS-CoV-2 Colorized scanning electron micrograph of an apoptotic cell (greenish brown) heavily infected with SARS-COV-2 virus particles (pink), isolated from a patient sample. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
Why Seroprevalence is Important
Checking Test Accuracy
To test the selected assay for specificity and sensitivity, it was first tested in 43 patients who were all positive for RT-PCR for the infection from nasopharyngeal or oropharyngeal swabs. The investigators used immunoassays based on chemiluminescence, with antibodies against the spike protein and nucleocapsid, respectively.
They found that about 94% of patients seroconverted for IgG, that is, produced IgG antibodies to the virus, at 22 days from the onset of symptoms. The sensitivity for IgG assay was about 97% at 22 days. Four patients failed to seroconvert, of which two had received a kidney transplant, and were on immunosuppressive drugs. One was over 90 years, and one patient had an acute psychiatric disease. Both the transplant patients did eventually seroconvert. The majority of immunosuppressed patients did seroconvert within two weeks. The corresponding figures for IgM seroconversion and sensitivity for IgM assay were 94% and 98%, respectively.
To test for specificity, the investigators examined blood samples from blood donors given before the start of the pandemic. They found that only 2/1,013 samples showed IgG positivity, for high specificity of 99.8%, and 6/1,492 samples were positive for IgM, for a specificity of 99.6%.
Screening for Antibodies
Having established the reliability of the assay, they tested the prevalence of the antibody in the San Francisco Bay Area in two groups of people who had a low probability of COVID-19. One group comprised 1,000 people who donated blood at blood banks in the area in March 2020 and had therefore been screened for any self-reported illness or abnormalities in the vital signs. They found 4/1,000 positive samples for IgG. IgM was not tested.
When they tested these for neutralizing antibodies using two other tests, three of the four were negative for both, and thus probably false positives. This left a seroprevalence of 0.1%, with a false positive rate of 0.3% that is in agreement with the reported specificity of the antibody test used.
The second group consisted of 387patients who were treated at various clinics or inpatient facilities under the UCSF Medical Center for illnesses other than COVID-19 between late March to early April 2020. There were 532 remnant samples from blood specimens drawn from these patients during their care.
There were five positives, all from one patient. The patient turned out to have had respiratory failure and ground-glass opacities on chest imaging but had not had RT-PCR for COVID-19. The seroprevalence was thus 0.26% in this group.
Only 23 of the samples could be tested for IgM, but all were negative.
Antibody timelines in COVID-19 Patients
The investigators then looked into the time trends of IgM and IgG in plasma, in 43 COVID-19 positive patients. They saw that both antibodies rose in parallel. Whether it was the median IgG, IgM or neutralizing antibody levels, when measured weekly, all were correlated with the intensity of disease. There was no significant difference.
Finally, they looked for an association between IgG and IgM antibodies with the presence of neutralizing antibodies against a pseudovirus carrying the SARS-CoV-2 spike protein. They compared the presence of the IgM and IgG with a plasma neutralizing antibody titer that was able to neutralize 80% of infective viral particles (NT80), in 54 plasma samples drawn from 22 of the 43 patients.
They found that in about 94% of cases, the NT80 was associated with IgG positivity, called positive percent agreement (PPA), while the negative percent agreement (NPA) was 75%. For IgM, PPA and NPA were 85% and 79%, respectively.
The appearance of neutralizing titers was in tandem with IgG and IgM antibodies rose in parallel with anti-spike IgM and anti-nucleocapsid IgG antibodies and could be correlated with the levels of IgG and IgM.
What Does This Show About Antibodies in COVID-19?
The investigators point out that this shows that seropositivity for these IgM and IgG antibodies can predict neutralizing capacity in vitro. This could be very helpful in identifying those COVID-19 patients who have recovered and who can donate convalescent plasma.
It is important to realize that in vitro neutralization may not correlate to protective immunity and that the effectiveness of convalescent plasma to treat COVID-19 is still unproven.
Another important finding is the very low seroprevalence of IgG antibodies in two separate groups of patients in a hospital in the San Francisco Bay Area in the study period. This is much lower than the limit of specificity for many immunological assays, and are lower than those found by many other community-based studies which show a higher seroprevalence in California. The lesson to be derived is the need to use a very specific test to carry out surveillance studies in a population where the prevalence of the condition is low.
Finally, the study concludes, the findings show “a very low likelihood of widespread cryptic circulation of SARS-CoV-2 in the Bay Area prior to March 2020, consistent with the low detection rate by direct viral testing of respiratory samples collected during that early time period.”
Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Journal reference:
- Ng, D. L., et al. (2020). SARS-CoV-2 seroprevalence and neutralizing activity in 1 donor and patient blood from the 2 San Francisco Bay Area. medRxiv preprint. doi: https://doi.org/10.1101/2020.05.19.20107482. https://www.medrxiv.org/content/10.1101/2020.05.19.20107482v1