The Indian Express
Covid is a ripe opportunity to strengthen the public health and social security system
It is not yet too late for India’s response to COVID-19 to recalibrate so that it serves community health and the public good in just this manner.
by Vivek DivanA decade ago, India demonstrated a health-related response that was acclaimed as a blueprint for how public health challenges can be successfully tackled. We seem to have forgotten (or dismissed) the fundamentals of that success already.
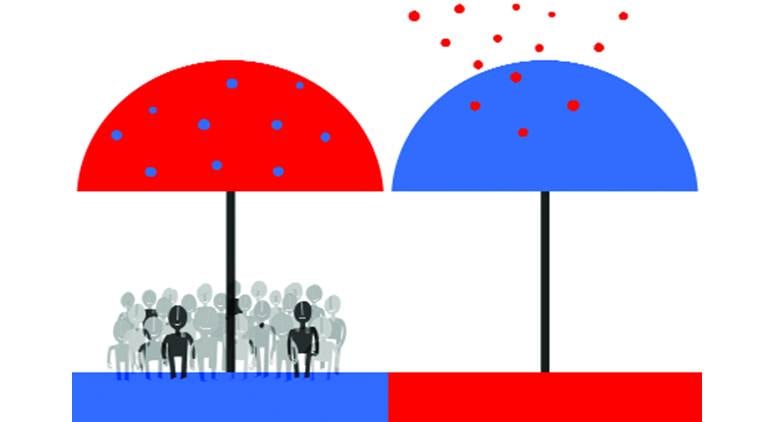
The decades-long response to HIV/AIDS fronted the following principles. First, dealing with epidemics requires placing the most marginalised and vulnerable at the forefront of any strategy. If their needs are met — whether in the form of access to information and services, or respect for their bodily, social and economic integrity — not only are their health outcomes more promising, but in all likelihood, the needs and health of others who are higher in the socio-economic ladder will also be met through such a thoughtful approach.
Shaping inclusive and nurturing health systems and social environments means that those delivering health are attuned to the realities of the vulnerable and marginalised, and can better serve their needs. It means fostering an environment of health and governance that those at the margins feel encouraged and safe to engage with. As a queer man who was vulnerable to HIV, I know how very distant a health system that shunned me and my ilk felt like in the 1990s. As a lawyer who has long worked on issues related to health, I saw how transformative it was to work with government bureaucrats, physicians, nurses, police, employers, and NGOs, who were open to conversations on sex, sexuality, illness and law, and how, over time, these dialogues fostered an enabling environment in the health sector, which began to reflect in policy, and in wider societal efforts to counter HIV.
Opinion | Lack of education, erosion of science has fuelled paranoia constructed around COVID-19
In the case of HIV, fostering such an environment meant sex workers, hijras, people living with HIV, drug users, men who have sex with other men were at the heart of health and public policy efforts. In the context of COVID-19, it means centering frontline personnel such as healthcare workers, sanitation workers, and the police, people with co-morbidities, senior citizens, and those whose lives are turned chaotic by harsh measures such as lockdowns — daily wage and migrant labourers, women and the urban poor.
Second, make the marginalised and vulnerable allies in this journey through a collective approach that listens to their needs and offers appropriate solutions. Do not treat them as subjects to be regimented, but partners to be empowered — bottom-up, not top-down. Strengthen them with reliable, relatable, destigmatising and evidence-based information and services, the rights to avail these, and a health and social system that does not castigate but welcomes.
This requires humility, a consciousness to know that whatever our expertise, we don’t have the solutions to health issues that are entwined with complex human realities. And that although those in the most serious predicaments may be lower in all the kinds of ill-conceived ways by which we measure social and human worth, they probably have insights that lead us together to solutions.
Opinion | The govt’s flagship health scheme has crossed 1 crore treatments, positively impacted lives
Third, leave one’s personal morality and the all-too-common human tendency to blame and vilify behind. This entails understanding how a disease transmits, but not faulting those who have it. Like with COVID-19, in HIV too an overwhelming majority of people have no idea that they are carriers.
Doing this in relation to HIV led to some extraordinary progress, including the maturing of a health bureaucracy for whom issues of human sexuality and sexual behaviour became routinely comfortable, one which was honest and empathetic about such issues, regularly at ease sitting with hijras and sex workers to listen and learn from them, and let such voices shape policy and practice, which became so much more reflective of ground realities, and therefore, more effective. Indeed, it was heartening to note that some of those who served in government at the peak of the HIV response are part of ICMR’s high-level technical committee of experts on COVID-19. They will have lessons to share from HIV. That advice should be heeded.
HIV was thwarted from ravaging India not by an intimidating top-down approach. It was contained because of an empowered community of affected citizens who demanded their health and related rights, and a place at the table as responsible solvers of the challenge, not docile recipients of directives. It was a community that demanded access to antiretroviral medication that made the government roll out and scale up a free programme that has saved and enhanced millions of lives. It was an active and diverse queer community that demanded an end to laws like section 377 which made them vulnerable to violence, unjust criminality and HIV that caused the law to be struck down. It was a vast swathe of citizens that worked on and obtained India’s first anti-discrimination law — the HIV/AIDS Act. It is this community which challenges illegitimate monopoly claims by big pharma to patent life-saving drugs that threaten to make medication unaffordable.
Admittedly, the response to HIV was disease-centric, strengthened with large sums of financing and human resources. Unfortunately, it failed to transform health systems more broadly, which should have been another positive outcome of such a resource-intensive effort. And undoubtedly, COVID-19 and HIV are different in their pathologies, causes, manifestations and impacts. Still, like the Basic Structure of India’s Constitution, there are some fundamentals which are true and work regardless of the nature of things.
Although the challenges of COVID-19 should not be dealt with in a disease-specific manner, this crisis is a ripe opportunity to strengthen the public health and social security system more fully, fortified by the humane and inclusive approaches that HIV has shown us. It is not yet too late for India’s response to COVID-19 to recalibrate so that it serves community health and the public good in just this manner.
This article first appeared in the print edition on May 27, 2020 under the title ‘HIV lessons for Covid-19’.
The writer heads the Centre for Health Equity, Law & Policy at ILS Pune