Precision scaffolds tailor biomaterials to promote wound healing
by Tami FreemanBiomaterials are used in the clinic as dressings that promote healing of wounds or burns. In addition to conventional wound dressings, scientists are developing skin substitutes containing patient-derived cells, as well as biomaterials that incorporate growth factors to stimulate and facilitate the healing process.
Once implanted, such biomaterials are exposed to the body’s immune response, particularly macrophages that can be either pro-inflammatory (M1) or pro-healing (M2) in type. While an initial inflammatory state is important for healing, prolonged inflammation is detrimental to tissue regeneration. Directing the immune response after implantation is thus a major challenge in the design of new biomaterials.
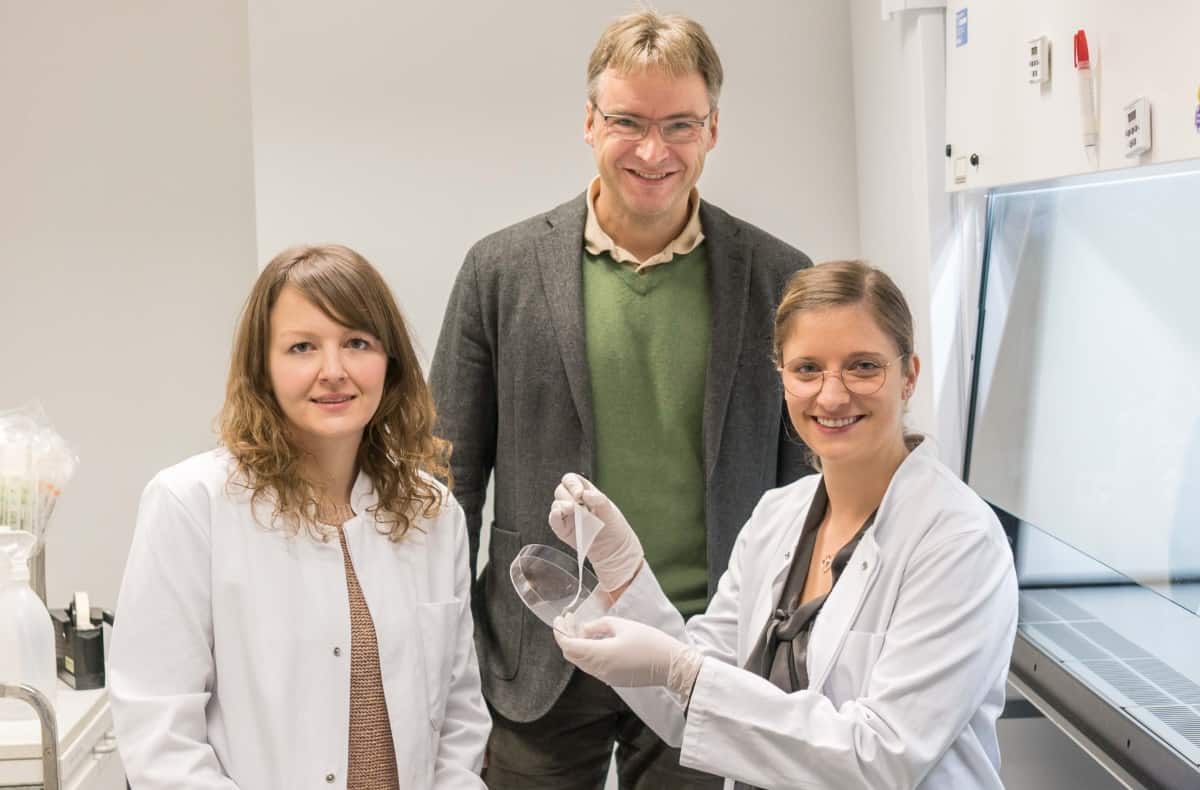
One way to drive macrophage type is by controlling their physical microenvironment, for example by tailoring the biomaterial geometry. With this aim, researchers at the University Hospital of Würzburg, have used melt electrowriting (MEW) to create high-precision 3D tissue scaffolds that cause human macrophages to differentiate towards the anti-inflammatory M2 type (Biofabrication 10.1088/1758-5090/ab5f4e).
“We wanted to determine the optimal scaffold geometry for the polarization of human macrophages into the M2 type,” explains senior author Jürgen Groll. “And when we found that macrophages on box-shaped scaffolds showed enhanced M2 polarization, we wanted to further determine the optimal pore size for them.”
Shape matters
Groll and colleagues used a customized MEW printer to fabricate 3D porous fibre scaffolds from the biocompatible polymer PCL. They created scaffolds with box-shaped, triangular, round and disordered geometries, and cultivated human-monocyte-derived macrophages on these scaffolds for seven days.

Scanning electron microscopy (SEM) revealed that cell morphology differed according to scaffold geometry. In particular, macrophages grown on box-shaped scaffolds developed an elongated shape and stretched across the pores.
Gene expression profiles after seven days growth also depended upon scaffold geometry, with box-shaped scaffolds appearing most promising for promoting macrophage differentiation towards M2 type. Macrophages cultivated on box-shaped scaffolds showed the highest expression of the M2 marker CD163, as well as the strongest downregulation of the pro-inflammatory cytokines IL-1β and IL-8 (which are released by M1 macrophages).
Guided by these outcomes, the team fabricated further box-shaped scaffolds with pore sizes from 40 to 100 μm and seeded them with macrophages. SEM images showed that, after seven days, macrophages cultivated in these scaffolds could stretch along single fibres and bridge across pores.
Decreasing the pore size increased the number of elongated macrophages with long cellular extensions. On scaffolds with 40 μm pores, more than half of the cells were elongated and had an average length of 80 μm. For scaffolds with 100 μm pores, only 20% of the cells were elongated, with a length of roughly 50 μm.
Gene expression
To study the impact of pore size on macrophage differentiation, the researchers examined gene expression from macrophages grown for seven days on scaffolds with varying pore sizes, as well as on 2D PCL films. All of the porous scaffolds triggered a significant decrease in M1 markers compared with the 2D film, suggesting an anti-inflammatory differentiation effect of porous scaffolds over the seven days.

Expression of M2-specific markers significantly increased on scaffolds with a pore size of 40–60 μm, but decreased on those with 80 or 100 μm pores. Macrophages on the 2D control showed minimal up- or down-regulation of M2 markers over the seven days.
The team also examined the macrophages’ phagocytic activity (ingestion of other cells or particles) by adding fluorescent beads to the culture medium. Phagocytic activity is important in initial healing, to act against pathogens that enter the wound. However, high activity is a characteristic of inflammatory M1 macrophages.
Fluorescence imaging showed that initial phagocytotic activity was far lower on scaffolds with smaller pores than on those with larger pores. After seven days, there was less phagocytic activity on the 3D scaffolds than on the 2D control.
“We showed that macrophages on 3D scaffolds have a higher phagocytotic activity on day one than on day seven and, therefore, would still be able to react against pathogens,” Groll tells Physics World. “However, the activity is lower on smaller pore sizes, which is beneficial because the risk of frustrated phagocytosis – where macrophages try to internalize something that is too large – is also diminished.”
Groll and co-authors conclude that scaffolds with precisely controlled pore sizes cause elongation of adherent human macrophages, along with a polarization towards M2 type – effects that were most pronounced for the smallest 40 μm pores. These findings could enable creation of pro-healing scaffolds solely through structural control, to improve biomaterials for tissue regeneration and wound healing.
The team has several follow-up studies ongoing and planned. “We are working on the development of other scaffold types that can also promote the elongation of macrophages,” says Groll, noting that this research was conducted within the ERC funded project Design2Heal. “In addition, we would like to investigate the biological mechanism for the elongation-driven polarization of macrophages. Finally, in vivo studies are planned.”